Diabetes and Oral Health
Diabetes Mellitus (DM) is a chronic health condition. The two most common types are Type I and Type II. Type I DM accounts for 5% to 10% [9], and Type II DM accounts for 85% to 90% [7] of the cases. Patients diagnosed with DM are often informed on the knowledge that this disease can have harmful effects on the eyes, kidneys, nerves, heart. But did you know diabetes can pose a serious threat to your oral health as well? Patients with uncontrolled diabetes are highly prone to developing periodontal diseases due to accelerated deterioration of the gingival tissues and alveolar bone. Periodontal disease can also reduce quality of life as it can cause pain, difficulty chewing, halitosis, and ultimately, tooth loss.
What is diabetes?
A patient is diagnosed with DM when their body’s mechanism of turning food into energy is impaired. The food eaten is broken down into glucose (sugar), which is released into the bloodstream. This leads to increase in sugar levels in the blood, and it signals the pancreas to release insulin. Insulin causes the blood sugar to be absorbed by the cells of the body to be used as energy. When the pancreas doesn’t make enough insulin or no insulin at all, an when the cells of body are not able to respond to insulin, the blood sugar stays in the blood stream and leads to serious health problems.
Types of Diabetes Mellitus
There are three main types:
- Type I Diabetes Mellitus: It is an autoimmune reaction where the body’s own immune system mistakenly destroys the insulin-producing (islet, or islets of Langerhans) cells in the pancreas. Diagnosed usually in children, teenagers and young adults.

- Type II Diabetes Mellitus: The body is not able to respond to insulin and therefore, cannot take up the glucose in the bloodstream for energy resulting in higher levels of glucose in the blood for a long period of time. It develops over and usually diagnosed in adults with sedentary lifestyle.
- Gestational Diabetes: It is diagnosed in pregnant women who have never had diabetes or were prediabetic. Usually, gestational diabetes does not stay after the birth, but it increases the risk of Type II DM later in life of the mother. The fetus is at risk of health problems if the mother is diagnosed with gestational diabetes. [11]

Why people with diabetes are more prone to periodontal disease?
Patients with uncontrolled diabetes and poor oral hygiene develop periodontal disease and this constitutes up to 22% of those diagnosed. [4] Uncontrolled diabetes means the blood glucose levels are not regulated properly, which results in the high glucose levels in the blood which weakens the white blood cells (WBC). WBC’s are the body’s main defense system against bacterial infections that can occur in the mouth. Since the immune system is weak, the gums are more prone to infections and les able to fight the bacteria resulting in periodontal disease over period. [13] Therefore, periodontal disease is considered a complication of diabetes. [6, 7, 9, 10]
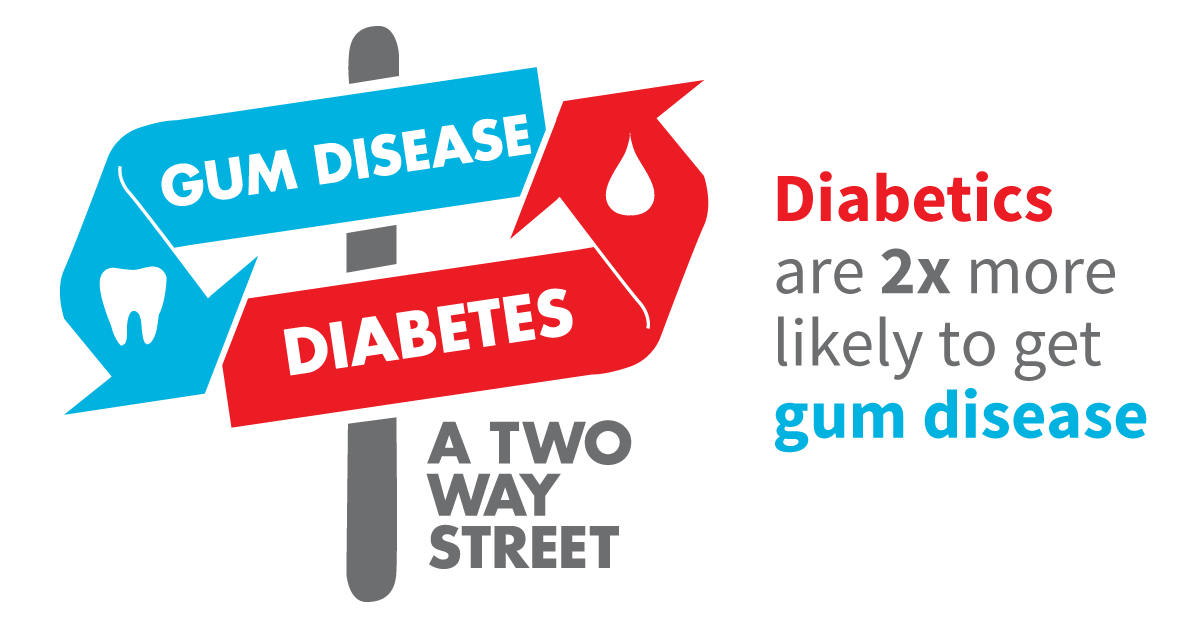
Research also suggests that the relationship between periodontal disease and diabetes is bidirectional. That means hyperglycemia affects oral health while periodontitis affects glycemic control (e.g., increased HbA1c). [1, 8, 15, 17]
A 2018 systematic review and meta-analysis update of a 2012 review established conclusions that periodontitis is associated with:
(1) higher HbA1c levels in persons without diabetes and persons with type 2 diabetes
(2) worsened complications from diabetes in people with type 2 diabetes
(3) a higher prevalence of complications in persons with type 1 diabetes. [6]
The study also found that periodontitis is associated with higher prevalence of prediabetes, and that severe periodontitis is statistically significantly associated with an increased risk of developing diabetes. [6]
Other studies have shown evidence that diabetes and smoking may have synergistic effect, and smoking, and diabetes are both risk factors for periodontitis. [5, 14]
Effects of diabetes on oral health
GUM DISEASE: A thin film bacterial layer constantly forms around everybody’s teeth. This layer must be removed by regular tooth brushing and flossing. If the plaque layer is not removed, they harden over time around and below the gums and is called calculus. The longer they remain the more it will irritate the gums and cause inflammation. This is gingivitis, which is, unhealthy or inflamed gums. If not treated, this may lead to periodontitis, which is an advanced gum disease that varies from mild to severe. The signs and symptom of gingivitis and periodontitis are mentioned in the table below. [3, 4, 12, 13, 16]



| Gingivitis | Gums appear red, and swollen. May bleed on brushing and flossing |
| Periodontitis | Red, swollen gums that bleed easily.
Gums have separated from the teeth. Presence of exudate(pus) when gums are pressed. Bad breath and bad taste in the mouth. Increased tooth mobility or migration. Changes in the way your teeth fit together when you bite Change in the way the partial dentures fit. |
Diabetes also causes blood vessels to thicken, which slows down the flow of nutrients and waste products from the tissues. Due to this, and weakening white blood cells, the body loses its ability to fight infections. Since periodontitis is a bacterial infection, patients with uncontrolled diabetes might experience more frequent and more severe gum disease. [13]
THRUSH (Candidiasis): Patients with uncontrolled diabetes often take antibiotics to make up for their low slow immune system, are especially prone to developing the fungal infection of the mouth and tongue. It is caused by the yeast Candida albicans (candida). It is a naturally occurring fungus in the mouth but takes advantage of the low immunity and causes infections. Wearing dentures constantly can also lead to fungal infections. The signs and symptoms of thrush are mentions in the table below. [3, 4, 12, 13, 16]

| Thrush (Candidiasis) | Painful, white and sometimes red patches on your gums, tongue, cheeks, or the roof of your mouth.
Patches may turn into open sores. May also cause burning or tingling sensations in the mouth. |
Your dentist may prescribe you with an antifungal mouthwash and gel.
DRY MOUTH (Xerostomia): It is caused by lack of saliva in the mouth which raises the risk for tooth decay, gum disease, and thrush. Saliva is made up of 99.5% water, and electrolytes, mucus, antibacterial compounds, and various enzymes. Saliva helps the to keep the teeth and mouth free from food particles and debris. It helps neutralize the acidic nature of the bacterial attack to prevent tooth decay. Patients with uncontrolled diabetes develop dry mouth, that can promote, tooth decay, and overgrowth of candida. The signs and symptoms of dry mouth are mentioned in the table below. [3, 4, 12, 16]

| Dry Mouth (Xerostomia) | Difficulty eating, chewing, swallowing, or talking.
Rough, and dry tongue. Dry feeling in the mouth, often or all the time. Cracked lips. Pain in the mouth. Mouth sores, and or fungal infections. |
BURNING MOUTH SYNDROME (BMS): There are many reasons a person can suffer from BMS. One of the reasons is uncontrolled blood glucose levels. The signs and symptoms of BMS are mentioned in the table below. [3]
| Burning Mouth Syndrome | Burning sensations in the mouth.
Bitter taste in the mouth. Dry feeling in the mouth. Symptoms may get worse throughout the day. |
IMPAIRED WOUND HEALING: Patients with uncontrolled diabetes, have impaired wound healing due to weak white blood cells and reduced flow of nutrients to the wound site due to thickened blood vessels. Due to this it takes longer for the extraction site or other oral surgery sites to heal. [12]

People with diabetes are 20 times more at a higher risk than non-smokers with diabetes to develop periodontitis and thrush. Also, smoking contains nicotine, which is a vasoconstrictor. That means it constricts the blood vessels, which impairs blood flow to the tissues, that in turn affects wound healing in that tissue area. [13]
How to take care of oral health if diagnosed
Patients with diabetes are highly prone to diseases that will harm the oral health. It is crucial to take steps to keep the mouth healthy by following excellent oral hygiene practices, paying attention to any changes in the tissue and teeth, and schedule an appointment with the dentist immediately if such changes occur.
If you have diabetes, then to prevent damage to your teeth and gums, you should take these steps of dental care seriously:
- Commit to managing your blood glucose levels. Measure your blood sugar levels everyday and manage to keep it within the target range with the help of your endocrinologist’s instructions, eating a healthier diet and exercising more. Maintaining your blood sugar level also helps your body’s immune system to fight of bacterial and fungal infections in your mouth. If your blood sugar level is controlled, it is less likely you will develop periodontitis.

- Brush your teeth at least twice a day and floss at least once a day. You should brush in the morning and at night, and after meals and snacks. You should use super soft-bristled toothbrush and fluoride containing toothpaste. Avoid brushing aggressively as this can irritate or cut the gums which can lead to infections. If you have arthritis or other problems that make brushing difficult, consider using electric toothbrush. Replace your toothbrush with a new one every three months.You should floss after every meal, ideally. It helps removes food debris and plaque from between your teeth and under your gums. You can used waxed floss as it is easier to pass between the teeth without cause irritation. You use floss holder for easier manipulation of the floss.If you wear a denture, partial or complete, you should clean it every day with a separate toothbrush and using appropriate denture cleaning gels and solutions. Ask your dentist to prescribe a suitable cleaning agent for your denture and proper instructions on how to clean the denture.
- Schedule regular dental appointments. Always give your dentist or periodontist your endocrinologist’s name and contact number for them to easily contact your doctor in case any questions or concerns arise.
 Give your dentist the full list of medicines and dosages of the medicines you are taking for the diabetes. This is to prescribe medicines that are least likely to interfere with medicines you are already taking.Before scheduling any treatment for periodontal disease or oral surgeries, ask your doctor to contact your dentist or periodontist about your overall health condition, the need to take any pre-surgical antibiotics, or if you need to change meal time and dosage of insulin (if you take insulin).
Give your dentist the full list of medicines and dosages of the medicines you are taking for the diabetes. This is to prescribe medicines that are least likely to interfere with medicines you are already taking.Before scheduling any treatment for periodontal disease or oral surgeries, ask your doctor to contact your dentist or periodontist about your overall health condition, the need to take any pre-surgical antibiotics, or if you need to change meal time and dosage of insulin (if you take insulin).
If your blood sugar is not in control, postpone non-emergency treatments. Acute infections (that develop quickly), such as abscess should be treated immediately and you should follow your dentist’s post-operative instructions strictly, as wound healing is slow in people with uncontrolled diabetes.
- Look for early signs of gum disease: Mention any abnormality you notice in your mouth to your dentist such as redness, bleeding gums, swelling, dry mouth, pain, burning, loose teeth, your denture stopped fitting correctly, soreness. If you wear braces, and if a wire or bracket cuts your tongue or mouth, you should contact your orthodontist immediately.

- Quit smoking: Ask your doctor for instructions on how to quit smoking as smoking increases the risk of periodontitis and loss of teeth in patients with diabetes. [2, 3, 4, 12, 13, 16]

Managing diabetes is a lifelong commitment, and that includes proper dental care. Your efforts will be rewarded with a lifetime of healthy teeth and gums.
There isn’t a cure yet for diabetes, but losing weight, eating healthier food, and exercising can really help. Taking medicine as needed, getting diabetes self-management education and support, and scheduling regular health care and dental appointments can also reduce the impact of diabetes on your life. [11]
References:
-
- Chapple, I. L. C., & Genco, R. (2013). Diabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. Journal of Clinical Periodontology, 40. doi: 10.1111/jcpe.12077
- Diabetes: Dental Tips. (2019). National Institutes of Health.
- Diabetes, Gum Disease, & Other Dental Problems. (2014, September 1). Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/gum-disease-dental-problems
- Diabetes and Your Smile. The Journal of American Dental Association. Retrieved February 3, 2020, from https://www.mouthhealthy.org/en/az-topics/d/diabetes
- Ganesan, S. M., Joshi, V., Fellows, M., Dabdoub, S. M., Nagaraja, H. N., Odonnell, B., Kumar, P. S. (2017). A tale of two risks: smoking, diabetes and the subgingival microbiome. The ISME Journal, 11(9), 2075–2089. doi: 10.1038/ismej.2017.73
- Graziani, F., Gennai, S., Solini, A., & Petrini, M. (2018). A systematic review and meta-analysis of epidemiologic observational evidence on the effect of periodontitis on diabetes. An update of the EFP-AAP review. British Dental Journal, 224(6), 427–427. doi: 10.1038/sj.bdj.2018.246
- Health, United States, 2017. (2017). National Center for Health Statistics.
- Kane, S. F. (2017). The effects of oral health on systemic health. Gen Dent, 65(6), 30–34.
- Kidambi, S., & Patel, S. B. (2008). Diabetes mellitus: considerations for dentistry. J Am Dent Assoc, 139. doi: 10.14219/jada.archive.2008.0364
- Lamster, I. B., Lalla, E., Borgnakke, W. S., & Taylor, G. W. (2008). The relationship between oral health and diabetes mellitus. J Am Dent Assoc, 139. doi: 10.14219/jada.archive.2008.0363
- Learn about Diabetes. Centers for Disease Control and Prevention. (2019, August 6). Retrieved February 3, 2020, from https://www.cdc.gov/diabetes/basics/diabetes.html
- Mark, A. M. (2016). Diabetes and oral health. The Journal of American Dental Association, 147(10), 852. doi: 10.1016/j.adaj.2016.07.010
- Oral Health Problems and Diabetes. (n.d.). Retrieved February 3, 2020, from https://my.clevelandclinic.org/health/diseases/11263-oral-health-problems-and-diabetes
- Pihlstrom, B. L., Michalowicz, B. S., & Johnson, N. W. (2005). Periodontal Diseases. The Lancet, 366(9499), 1809–1820.
- Sanz, M., Ceriello, A., Buysschaert, M., Chapple, I., Demmer, R. T., Graziani, F., Vegh, D. (2018). Scientific evidence on the links between periodontal diseases and diabetes: Consensus report and guidelines of the joint workshop on periodontal diseases and diabetes by the International diabetes Federation and the European Federation of Periodontology. Diabetes Research and Clinical Practice, 137, 231–241. doi: 10.1016/j.diabres.2017.12.001
- Standards of Medical Care in Diabetes–2014. (2018). Diabetes Care.American Diabetes Association., 41(1). doi: 10.2337/dc18-Sint01
- Ziukaite, L., Slot, D. E., & Weijden, F. A. V. D. (2018). Prevalence of diabetes mellitus in people clinically diagnosed with periodontitis: A systematic review and meta-analysis of epidemiologic studies. Journal of Clinical Periodontology, 45(6), 650–662. doi: 10.1111/jcpe.12839


